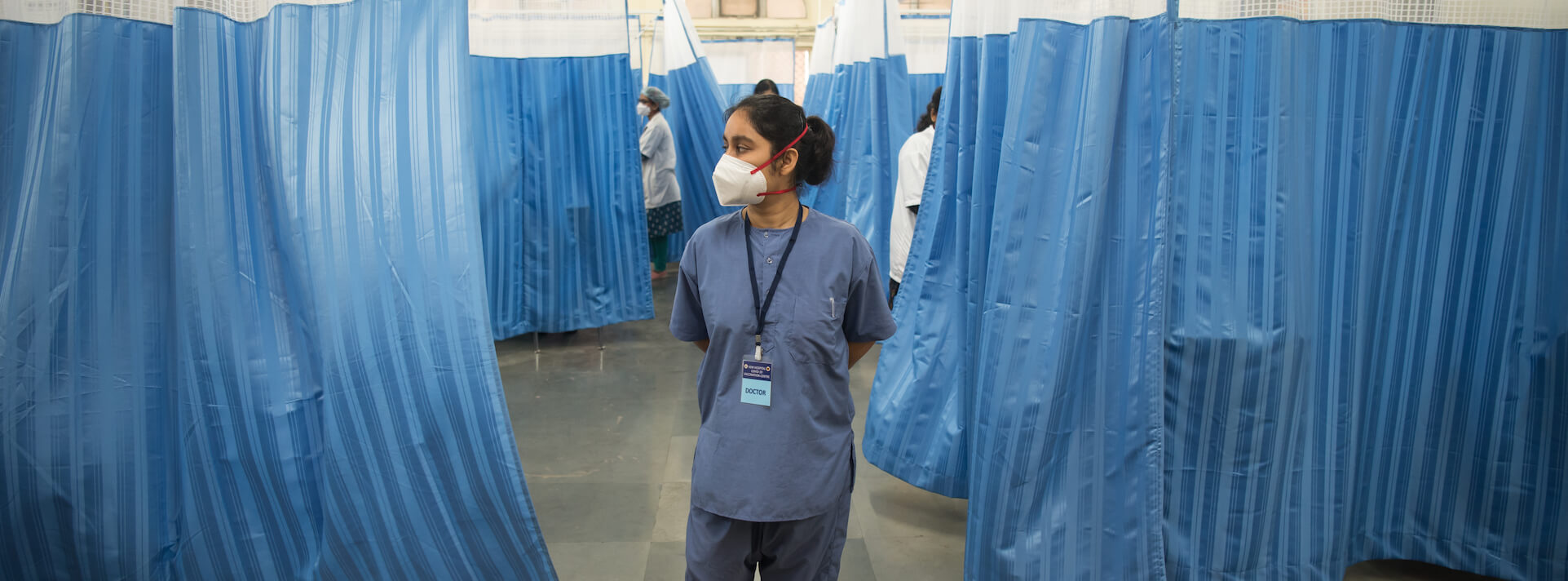
Although global efforts had been underway to improve digital health solutions at scale, it was the COVID19 pandemic that brought the necessity of digital health solutions into sharp focus.
Some solutions demonstrably help health systems extend remote care in less accessible areas, monitor health status of patients, make public health decisions based on population health surveillance data, and improve communication within healthcare providers spread across the care continuum.Furthermore, bringing down healthcare costs for the public and improving the efficiency of care service delivery at the last mile are critical for the success of digital health solutions.
Despite its potential to move the needle on essential healthcare coverage for the underserved, the field of digital health faces challenges around sustainability, scalability, and integration of solutions within health systems. One of the underlying causes is the lack of funding.
Health systems in low- and middle-income countries (LMICs) have historically struggled with financing. For domestic innovators and solution developers in LMICs, having a consistent flow of funding for all functions across the value chain is a chronic Achilles’ heel. High per unit manufacturing costs, cash flow crunch, high cost of change management, and low demand from healthcare providers make innovation and solution development a perilous enterprise.
Innovative financial tools
Last September in London, Sattva brought together philanthropists, impact investors, frontline organisations, academics, and ecosystem builders to explore trends, opportunities, and challenges for digital health for the Global South. Impact financing expert, Audrey Selian, commented that digital health solution providers are often able to secure some grant money and investments from family and friends to start off. They may then onboard some impact investors to secure a few hundred thousand dollars. But this marks the funding precipice. After this it becomes harder to expand, as very little funding is available.
According to social entrepreneur and impact investor Steven Serneels, venture capitalists find the medtech space to be risky, especially for the underserved areas, making it all the more important for solution developers to de-risk such investments through non-financial partnerships. For instance NGOs can be engaged for technical assistance, capacity building, and patient education – and securing grant funding.
All roads, therefore, point to blended finance.
In the impact funding space, instruments like volume guarantees and returnable grants can address issues arising from high capital expenditure and limited manufacturing volume – leading to higher per unit costs. On the other side of this exchange, small-scale healthcare providers may have to deal with the high cost of digitalisation and instituting change management. To address this problem, concessional loans or low-cost debts could be of value.
Volume guarantees to reduce per unit cost and capital expenditure
Solutions like wearables, point-of-care devices, and tele-ICUs have the potential to improve health monitoring, screening, and care delivery. Some of these solutions have high capital expenditure or unit production cost. In the absence of comprehensive health insurance on a mass scale, the bulk of medical expenditure is borne by patients themselves and the public system. For example, the capital expenditure to set up a 10 bed tele-ICU in India is $53,000 (10 Bed ICU n.d).
Any technological service adds to the service fee and may face resistance from healthcare providers and consumers. Niramai, the AI/ML-based breast cancer screening solution has already reduced screening cost by 60%. However, the current cost of $22 per test might still be unaffordable in the underserved areas. This can be reduced with higher production volumes.
A volume guarantee can provide the necessary price and volume commitment to the manufacturing company and serve as a shock absorber in case of market failures. In a volume guarantee agreement the manufacturer agrees to sell the product at or below the agreed price for the term of the agreement and manufacture an agreed minimum volume of products available for each year of the guarantee.
Returnable grants for addressing cash flow issues
Healthtech startups often face a cash flow crunch triggered by high upfront costs and working capital, which limits their ability to scale up in these markets. Startups working in the public sector also experience long sales cycles and complicated tendering processes. Returnable grants can bridge the funding gap by providing upfront capital at zero interest. A returnable grant, unlike a zero-interest loan, is not a balance sheet transaction, and is treated as income (not as a liability).
It is a moral obligation on the recipient to return it and no legal recovery actions can be taken by the financier in case of default. It also does not build a credit history. Alternatively, a zero-interest loan instrument can also be looked at. Occasionally, the instrument can be structured in a way where the obligation to return the money can be waived off under the precondition of achieving certain health outcomes.
Low-cost or concessional debt financing for change management costs
Given the capital-intensive nature of the business and input costs, most small-to-mid-sized hospitals operate at very low margins. Once the hospital is set up, achieving operational breakeven can take many years. Low margins inhibit hospitals from investing additional capital for digitalisation. The cost of change management combined with a lack of clear understanding of the value proposition inhibits private healthcare facilities from going digital.
While grants can be structured to support digitisation of public and charitable health facilities; for private hospitals, especially low cost facilities, that are willing but unable to invest upfront capital for digitalisation, low-cost or concessional debts can provide easier and affordable avenues.
Concessional loans offer interest rates lower than market rates. They have lenient terms, such as extended grace periods (during which only interest or service charges are due) and interest holidays. Concessional loans generally have longer repayment schedules as compared to traditional loans. Soft loans can be provided to healthcare facilities to help set up their digital infrastructure. These loans can also be availed of when the project is not eligible for grants, or the beneficiary cannot afford traditional loan rates.
Social Impact Bonds for driving citizen demand and adoption of digital health solutions
Poor health-seeking behaviour among citizens, the prevalent digital divide, and the lack of foundational digital infrastructure have added to the challenges in accessing and adopting digital health solutions in rural and inaccessible regions. This low uptake can also be attributed to lack of awareness and low perceived value of the benefits of using digital health solutions in improving overall health and well-being. This can result in a lack of willingness to pay for digital health products and services, in spite of the ability to do so.
In other cases, citizens from the lower and lower middle income strata are unable to pay for digital health services, given their socio-economic conditions. Impact bonds are concerned with the outcomes instead of inputs and activities. A results-based financing instrument such as a social or development impact bond along with grants can help improve health-seeking behaviour, promote digital inclusion, and increase awareness in the community by focusing on conveying a clear value proposition and building citizen capacity to leverage digital health solutions.
The provision of upfront capital can also help design appropriate interventions and onboard necessary partners without having to worry about returns. Due to the nature of the contract, the focus would be on improving the overall health-seeking behaviour, increasing receptiveness and acceptability of digital health solutions, and overall improvement of citizen health outcomes, especially for non-communicable diseases such as cardiovascular disease, diabetes, and mental health issues.
Concluding reflections
As technology continues to advance at an exponential rate, it is easy to imagine the potential for digital solutions to close the health gap amongst underserved communities. But a number of challenges still exist, particularly in the Global South. By taking a fresh look at how digital health is financed we have the potential to unlock capital at the scale that is commensurate with the needs of these underserved communities. A deeper dive into digital health in the Global South can be found at the Sattva Knowledge Institute.
At Sattva Knowledge Institute, Ritika Ramasuri is a research associate at the health practice, Daniel Rostrup is the regional business development lead for Europe, and Granthika Chatterjee is an engagement manager at the health practice.